“7 Shocking Truths About Lyme Disease: The Hidden Epidemic Destroying Lives”
Lyme Disease: The Hidden Epidemic
A Comprehensive Guide to Understanding, Prevention, and Living with Lyme
The Silent Invader: Understanding Lyme Disease
Imagine this: You’ve just returned from a beautiful hike through the woods, feeling refreshed and connected with nature. Weeks later, you start experiencing strange symptoms – fatigue that doesn’t go away with rest, joint pain that migrates around your body, and perhaps a mysterious rash. What you might be facing is Lyme disease, an illness that’s often misunderstood, frequently misdiagnosed, and can dramatically alter lives.

Nature’s beauty comes with hidden risks – ticks carrying Lyme disease thrive in wooded areas
Lyme disease isn’t just another illness; it’s a complex bacterial infection that can mimic hundreds of other conditions. What starts as a tiny tick bite can evolve into a multi-system disorder affecting the nervous system, heart, joints, and more. The Centers for Disease Control and Prevention (CDC) estimates that around 476,000 Americans are diagnosed and treated for Lyme disease each year, but many experts believe the actual number is much higher.
Why Lyme Disease Is So Misunderstood
Lyme disease presents unique challenges for patients and doctors alike. The bacteria responsible (Borrelia burgdorferi) is a master of disguise – it can change its surface proteins to evade the immune system, hide in tissues where antibiotics have difficulty reaching, and even form protective biofilms. This adaptability explains why some patients struggle with persistent symptoms even after treatment.
In this comprehensive guide, we’ll walk through every aspect of Lyme disease – from its history and biology to diagnosis controversies and cutting-edge research. Whether you’re a concerned parent, an outdoor enthusiast, or someone navigating the challenges of chronic Lyme, this article aims to be your definitive resource.
The Biology Behind the Bite
At the heart of Lyme disease is a remarkable yet troublesome bacterium: Borrelia burgdorferi. This spiral-shaped bacterium (a spirochete) is transmitted primarily through the bite of infected black-legged ticks, commonly known as deer ticks.
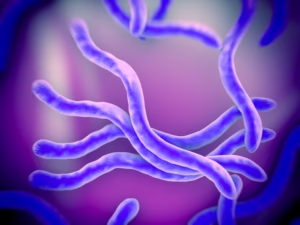
Borrelia burgdorferi bacteria under electron microscope
What makes this bacterium particularly challenging is its complex life cycle and sophisticated survival mechanisms:
- Shape-shifting abilities: Borrelia can change its outer surface proteins to evade the immune system
- Stealth mode: It can hide in collagen-rich tissues and even cross the blood-brain barrier
- Persistent forms: When threatened (like by antibiotics), it can transform into dormant cyst forms
- Co-infections: Ticks often carry other pathogens that can complicate diagnosis and treatment
Not Just a Summer Problem
While most infections occur between May and August, ticks can be active whenever temperatures are above freezing. Climate change has extended the active season for ticks in many regions, making Lyme a year-round concern in some areas.
Recognizing the Signs: Symptoms Across the Spectrum
Lyme disease is often called “The Great Imitator” because its symptoms can resemble so many other conditions – from fibromyalgia and multiple sclerosis to chronic fatigue syndrome and autoimmune disorders. This is why understanding the full spectrum of possible symptoms is crucial.
✓ Early Stage Symptoms
- Erythema migrans rash (bull’s-eye rash)
- Flu-like symptoms without respiratory issues
- Fatigue and malaise
- Headache and neck stiffness
- Swollen lymph nodes
- Muscle and joint aches
✓ Intermediate Stage Symptoms
- Severe headaches and neck stiffness
- Facial palsy (loss of muscle tone)
- Heart palpitations or irregular heartbeat
- Dizziness and shortness of breath
- Nerve pain and numbness
- Arthritis with severe joint pain
✓ Late Stage Symptoms
- Chronic arthritis and joint swelling
- Severe cognitive difficulties
- Neuropathy (nerve damage)
- Sleep disturbances
- Heart rhythm abnormalities
- Mental health challenges


The classic bull’s-eye rash (erythema migrans) appears in 70-80% of infected persons
Critical Insight
Approximately 20-30% of infected individuals never develop the telltale bull’s-eye rash, which is why Lyme often goes undiagnosed in its early stages. If you experience flu-like symptoms during tick season without respiratory symptoms, consider Lyme as a possibility.
The Diagnostic Dilemma
Diagnosing Lyme disease remains one of the most challenging aspects of this illness. Current testing methods have significant limitations, leading to both underdiagnosis and overdiagnosis.
The standard two-tiered testing protocol (ELISA followed by Western Blot) recommended by the CDC misses up to 50% of early Lyme cases. This happens because:
- It takes 4-6 weeks for antibodies to develop
- Antibiotic use early in infection can suppress antibody production
- The bacteria can suppress the immune system
- Different strains may not be detected by standard tests
Emerging Diagnostic Technologies
Researchers are developing promising new approaches including PCR tests that detect bacterial DNA, T-cell tests that measure immune response, and even techniques using nanotechnology to detect the bacteria directly. While not yet widely available, these offer hope for more accurate diagnosis in the future.
Navigating Treatment Options
Treatment for Lyme disease varies significantly based on how early it’s caught, the symptoms present, and whether co-infections are involved. The standard approach recommended by the Infectious Diseases Society of America (IDSA) involves:
Early Localized Lyme
14-21 days of oral antibiotics (usually doxycycline, amoxicillin, or cefuroxime)
Early Disseminated Lyme
21-28 days of oral or intravenous antibiotics for neurological symptoms or heart issues
Late Lyme Disease
28 days of oral or IV antibiotics, with potential retreatment if symptoms persist
The Controversy of Chronic Lyme
Approximately 10-20% of patients continue to experience symptoms after standard antibiotic treatment, a condition sometimes called Post-Treatment Lyme Disease Syndrome (PTLDS). This area remains highly controversial, with some doctors advocating for extended antibiotic treatment and others warning of serious risks without proven benefits.
Many patients with persistent symptoms turn to integrative approaches that may include:
- Herbal protocols (such as Japanese knotweed, cat’s claw, and andrographis)
- Dietary changes to reduce inflammation
- Detoxification support
- Addressing co-infections like Babesia and Bartonella
- Managing immune dysfunction and nervous system regulation
A Personal Journey: Living with Lyme
“I was an active 32-year-old teacher when my health began to unravel. First came the crushing fatigue – I’d sleep 12 hours and wake up exhausted. Then the joint pain started, migrating from my knees to my wrists to my shoulders. My doctor ran test after test, but everything came back ‘normal.’ It took 18 months and seven doctors before I finally got my Lyme diagnosis. That was five years ago, and while I’ve made significant progress, I still have days where getting out of bed feels like climbing a mountain. My advice? Trust your body, keep searching for answers, and know you’re not alone in this fight.” – Sarah J., Lyme survivor
Trusted Resources for Lyme Disease Information
- CDC – Lyme Disease Homepage – Official guidelines and statistics
- LymeDisease.org – Advocacy, research, and patient support
- International Lyme and Associated Diseases Society (ILADS) – Physician education and guidelines
- Columbia University Lyme and Tick-Borne Diseases Research Center – Cutting-edge research
- Global Lyme Alliance – Research funding and education
- NIH – Continuing Controversies in Lyme Disease – Scholarly article
Hope on the Horizon
While Lyme disease presents significant challenges, there are reasons for optimism. Research is advancing on multiple fronts – from new diagnostic methods to innovative treatments and even vaccine development. Increased awareness is helping patients get diagnosed earlier, and the medical community is gradually acknowledging the complexities of persistent Lyme symptoms.
Whether you’re a patient, caregiver, or simply concerned about tick-borne diseases, knowledge is your best defense. Stay vigilant about prevention, listen to your body, and advocate for your health. With continued research and awareness, we can turn the tide against this complex illness.
Share this content:





